With fall festivities in full swing and Halloween fast approaching, physicians in North Texas have broken down traditional activities into low, moderate, and high-risk categories according to CDC guidelines.
“Some traditional Halloween festivities need to be modified this year to avoid high-risk activities involving close contact, but there are still plenty of fun holiday activities to enjoy with your kids,” said Dr. Beth Kassanoff, Vice Chair of the North Texas Medical Society Coalition and President-Elect of the Dallas County Medical Society. “Continue to stay physically distanced, wear a cloth or disposable surgical mask, and wash your hands, but have fun with the holiday.”
As with all activities during the COVID-19 pandemic, participants should wear a cloth face covering, maintain physical distance, and wash their hands frequently while participating in any of these activities. Additionally, wearing a cloth face covering along with a traditional costume mask over or under it should be avoided.
Low-Risk Activities:
- Carving and decorating pumpkins with members of your immediate household or with friends at tables 6-10 feet apart, separated by household.
- Halloween scavenger hunts with members of your immediate household.
- Decorating your home.
- A virtual Halloween costume contest with your school, friends, and/or family.
- A physically distanced Halloween movie with an outside screen and projector, or a family movie night inside with the members of your immediate household.
- A pinata at home with members of your immediate household.
Moderate-Risk Activities:
- A small group (less than 10 people) outdoor costume parade while maintaining physical distance and wearing a cloth face covering.
- Individual goody bags set up on an outside table for grab-and-go trick or treating. Consider leaving hand sanitizer for added safety.
- Visiting pumpkin patches while maintaining physical distance and wearing a cloth face covering.
High-Risk Activities:
- Traditional trick or treating door-to-door.
- ‘Trunk or Treat’ events and Fall Festivals and carnivals.
- Haunted Houses.
- Hayrides.
- Outdoor gatherings that do not allow for physical distancing or any indoor parties or events with individuals outside your immediate household.
Some steps you can take to mitigate concerns might include:
- Get your flu shot at least two weeks before Halloween.
- Use hand sanitizer regularly and avoid touching your face.
- Wear a cloth face covering if you are participating in any Halloween activities with people other than those living in your home.
- Wash your hands well before eating.
- Do not participate in activities with other people if you are sick or have been exposed to COVID-19.
About North Texas Medical Society Coalition:
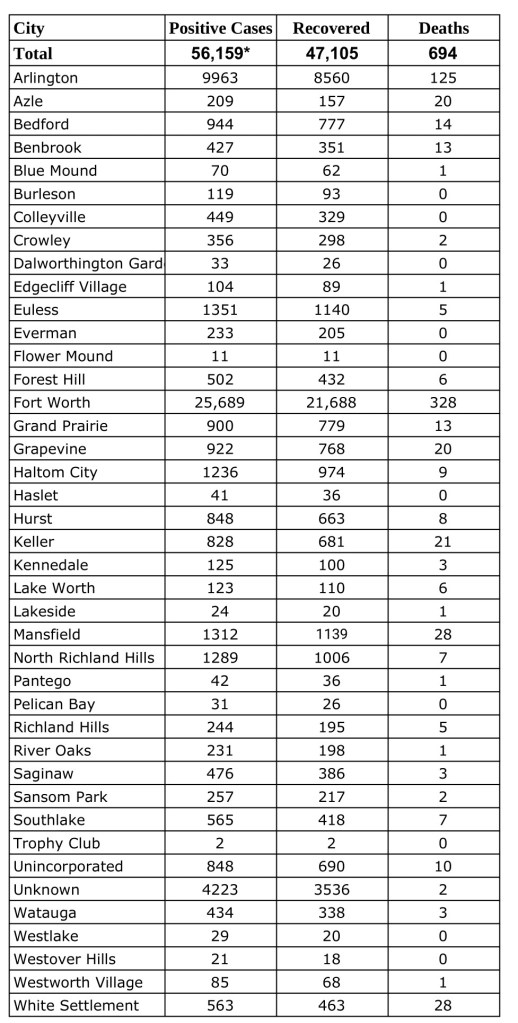
The NTMSC represents more than 11,500 physicians in the communities of Collin-Fannin, Dallas, Denton, Grayson, and Tarrant County. Founded in 2020, the NTMSC works with community healthcare partners, including public health departments, hospitals, and business leaders, to advise on medical recommendations to serve the health care needs of the residents of North Texas.