Feature Article
By Allison Howard Hunter
This article was originally published in the November/December 2025 issue of Tarrant County Physician.
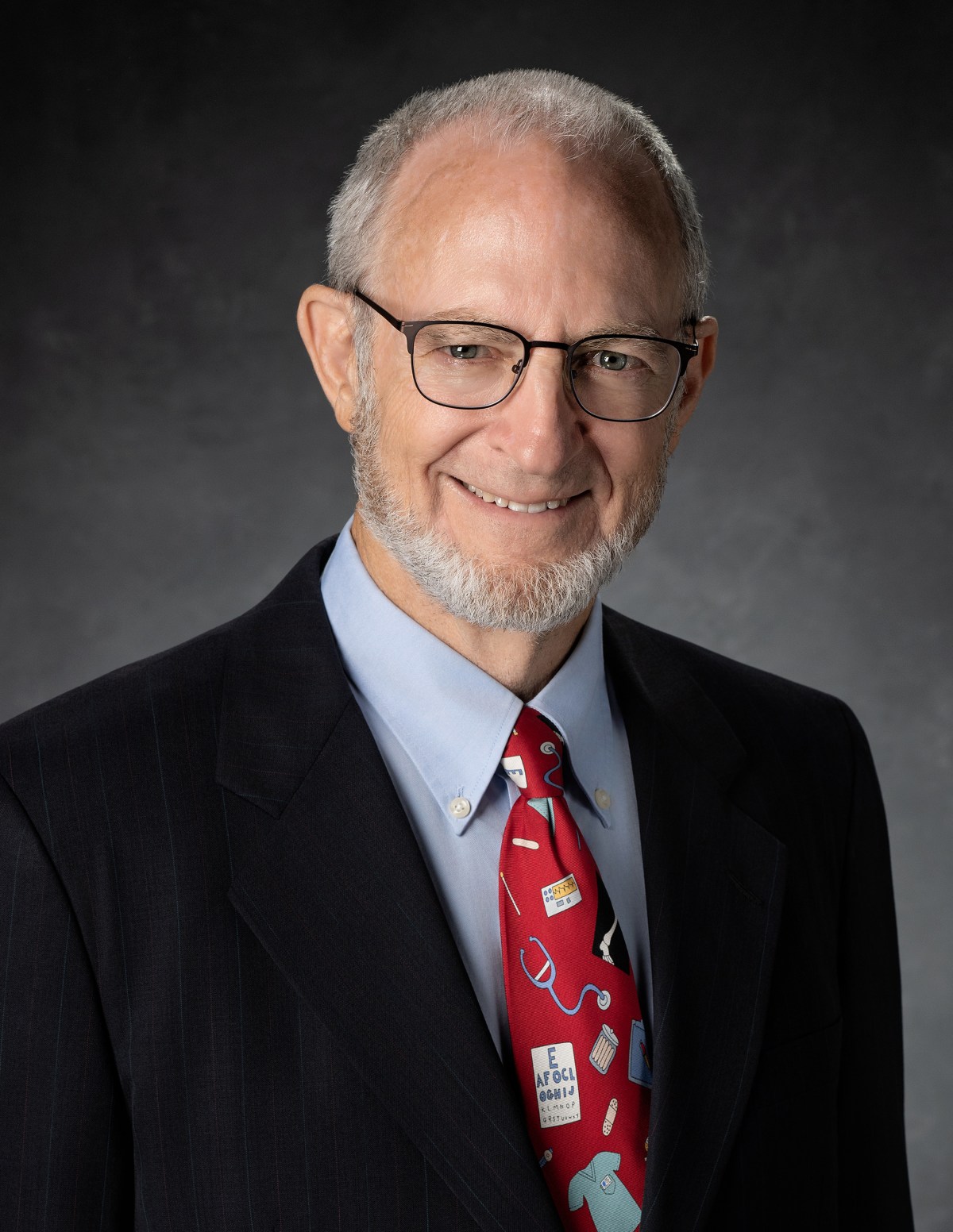
When asked about the best aspect of practicing medicine, Dr. David Capper doesn’t miss a beat. “It’s the people,” he explains. “I think it really just boils down to the opportunity to have in-depth relationships with people.” This makes perfect sense when you look at the trajectory of Dr. Capper’s career—it’s always about the people, whether it’s the unhoused, the underserved, or the dying. From his involvement in street medicine to his longtime work in hospice care, Dr. Capper’s passion for people has led his peers to select him as the 2025 Gold-Headed Cane recipient. For those who know him, it doesn’t come as a surprise.
“David truly embodies the spirit of the Gold-Headed Cane,” says 2024 Gold-Headed Cane recipient Stuart Pickell, MD, a longtime friend of Dr. Capper’s. “I once heard of a patient he treated for skin lesions caused by an arthropod infestation. Not only did David provide medical care, but he also arranged—and personally paid—for the patient’s home to be exterminated. That story captures who he is at his core: physician, colleague, advocate, educator, ethicist, disciple.”
Dr. Capper’s life can be defined by many excellent things, but he defines himself by what is most important to him: his faith in Jesus. As a longtime Christian, Dr. Capper says his motivations ultimately come from his desire to honor God by serving others. He cites Matthew 5:16 as his guiding scripture: “Let your light shine before others, that they may see your good deeds and glorify your Father in heaven.” (NKJV)
He is humbled to receive the Gold-Headed Cane, which he has a unique tie to: his father, Robert Capper, MD, himself received the recognition in 2005.
“It’s not something you strive for,” says Dr. Capper. “What I thought about the Gold-Headed Cane over the years is that it’s a recognition of the peers of a physician whose life was committed to the profession and those professional values. And so, it’s very humbling, and it’s honoring.”
Dr. Capper has long had a passion for service, but he wasn’t always sure that medicine would be his medium. Though his father was a physician and his mother a nurse, he didn’t decide to pursue medicine until he was near the end of his collegiate career.
“I had an extremely high regard for my father and his peers,” he says. “The people that I was introduced to through my parents that were physicians were of the highest integrity, and I thought that’s the way physicians all were. And I didn’t quite see myself in that same category.”
It wasn’t until an emergency appendectomy between his junior and senior years of college that his path became clear. In a way, this was a blow—Dr. Capper was the captain of his football team, and he had recently gotten an All-American honorable mention, yet he would not be able to play the first half of the season. But being forced to slow down gave him the opportunity to spend a lot of time praying about his future. By the end of his stay, Dr. Capper felt a clear calling to become a physician in spite of his reservations. And instead of being intimidated by the excellence of the physicians he knew, he used it as a standard to strive for.
After Dr. Capper completed his undergraduate degree in liberal arts from Austin College and fulfilled his prerequisites, he began his tenure at the University of Texas Medical School at Houston. This was an enriching time that opened Dr. Capper’s eyes to the many possibilities of medicine.
He graduated from medical school in 1982 and was accepted into Good Samaritan Hospital’s internal medicine residency program in Portland, Oregon. It had a multidisciplinary pain program and was home to one of only two hospices in the state, both of which Dr. Capper credits as being formative to his education.
Throughout his medical training, Dr. Capper did extensive mission work, with the goal of eventually working in foreign medical missions. During this time, he met his wife, Dianne, who shared his passion for ministry. When he completed his residency, they planned to pursue mission work together, but a number of life circumstances kept them from taking the leap.
They ended up moving to Tyler, Texas, where Dr. Capper filled in as an emergency room physician. The family eventually came to Fort Worth, where he worked in the Harris Methodist Hospital Emergency Department and then joined E. Richard Holden, MD, a hematologist who needed help in his practice. Ultimately, Dr. Capper pivoted his ministry mindset to a local one—for the most part. Though he never went into foreign mission service full time, he has participated in over 30 short-term mission trips, the majority of which had a medical basis.
In the years since, Dr. Capper has worked in a variety of positions. He would not consider himself a traditional internist—he has a background in emergency medicine, pain management, geriatrics, cardiology, and palliative care that have played extensive roles in his career.
“I don’t know what I’m going to do when I grow up,” he says, laughing. “I’ve worn so many different hats and continue to do so.”
Throughout his extensive career, Dr. Capper has been heavily involved in medical education for both students and residents, was among the founders of a hospitalist program, worked in private practice, had a leadership role in an independent physician association, was the medical director of a PPO, and served as the medical director of one hospice program and CEO of another. He was among the founding members of a charitable clinic and helped to start JPS’s street medicine program, serving as their de facto medical director in its earliest years. He has worked as a nocturnist and helped to start several medical organizations.
Through the many roles he has held, one he has continually been drawn to is the critical but challenging practice of palliative and hospice care. While there is nothing easy about this field, he values the opportunity to help complex patients manage their conditions and terminal patients pass their last days with the greatest possible dignity and comfort.
Currently, Dr. Capper serves as the CMO of Community Healthcare of Texas, where he also oversees both their hospice and supportive care programs. He is on the faculty of both the TCU Burnett School of Medicine and the Texas College of Osteopathic Medicine (TCOM).
Dr. Capper has been impacted by many people throughout his career, but his greatest support has always come from Dianne, who has worked in ministry alongside him—all while raising their six children and, for a time, their foster daughter.
“I can’t have this conversation without talking about my wife,” Dr. Capper says. “She has supported me and managed our family in my life of craziness; it’s really remarkable.”
He is also grateful for his many siblings and their spouses—he is one of seven—and his parents for the impact they have had on him.
“I have a phenomenal family,” Dr. Capper says. “And you talk about influence on your life. . . . There’s a natural motivation when you have such great people who are encouraging you to do well.”
He views his parents as his ultimate medical heroes and says that their hearts of compassion were critical in the formation of his own worldviews. There are many other mentors and friends he would like to acknowledge for the impact they’ve had on him, and a few are the late John Richardson, MD; Drew Ware, DO; Michael Ross, MD; John Burke, MD; and Bob Keller, MD.
Dr. Capper is grateful for the impact his colleagues have had on his life, and many of those he has worked alongside over the years return the sentiment.
“David is a solid, conscientious physician, and I always felt secure knowing that he was helping my patients when I was away,” says Greg Phillips, MD, a friend and former colleague. “His work in our community helping the underserved and uninsured is without equal.”
Dr. Capper stresses that for patients who are underserved, it is critical to meet them where they are.
“The old saying goes that healthcare is local, right?” he says. “And it’s also true for disenfranchised communities.”
After Dr. Capper began practicing medicine in Texas, he and a group of dentists, physicians, and nurses worked together to start Beautiful Feet’s charitable clinic. It was 1988; JPS only had one central clinic, and the Fort Worth city-run clinics were in the process of being shut down, leaving a gaping hole in the community. The new clinic saw its first patients in 1989, and they have been going strong since. Dr. Capper has served as the group’s volunteer medical director since their doors opened.
“Dr. Capper has been leading [the] . . . clinic through Beautiful Feet Ministries for over 40 years, targeting the homeless and poor living in the Historic Southside of Fort Worth,” says Sarah Myers, Beautiful Feet Ministries co-director. “Through this clinic, countless people have benefited from Dr. Capper’s expertise and compassion.”
Approximately 80 percent of the clinic’s patients are unhoused, which creates unique challenges for continuation of care. His longtime work with this population made Dr. Capper an ideal fit for heading up JPS’s work in street medicine. Later brought on to oversee the palliative care program at JPS, his role grew from working as the volunteer medical director to eventually becoming the staff medical director of their unhoused program.
Though he stepped away from the position in 2022, Dr. Capper is proud of the strides JPS has made in street medicine.
“When we were able to get the 1115 waiver grants—well, I’m not proud of a lot of things, but I am proud of what we were able to structurally do with that,” says Dr. Capper. “And that allowed us to create a program that really addressed the needs of Tarrant County homelessness.”
Though there is a great need for medical care among the unhoused, Dr. Capper has had a broader outreach than that. He helped to form Project Access Tarrant County (PATC), Tarrant County Academy of Medicine’s (TCAM) program that provides specialty charitable care for those who have no resources outside of emergency rooms and primary care charity clinics. He has been on the PATC board since the organization was formed in 2011.
“Dr. Capper was integral to the creation and success of Project Access,” says PATC Director Kathryn Keaton. “His knowledge of charitable care is second to none and is only exceeded by his passion for accessible, comprehensive care for every individual in Tarrant County.”
Dr. Capper is heavily involved in charity care, but he still makes time to focus on a sister cause: medical ethics. He has been on a number of ethics committees, including TCAM’s ethics consortium, and he currently chairs the ethics committee at Medical City Fort Worth.
Because of his work in palliative and hospice care, this has continued to be a significant focus throughout his career.
“You have a lot of potential ethical conflicts in this world,” he says, “so I started going to conferences 20 years ago and then eventually entered a master’s program in biomedical ethics.”
He graduated with his master’s from Trinity International University this past December, and he plans to keep teaching medical ethics not only to physicians but to the public at large.
“So many of these conflicts that we deal with in clinical ethics, they come back to just people living their lives,” Dr. Capper says. “How many of these ethical conflicts could be avoided if people only took a knowledgeable approach to their own advance care planning?”
Like many things, Dr. Capper believes it comes back to education—one of his greatest passions.
Dr. Capper knew he liked to teach early in his career. When he had an extended year in his residency as the chief resident, it was a heavily teaching-focused position. He loved sharing with and learning from other doctors to make the group better as a whole.
When he moved to Fort Worth, teaching at TCOM—which his father had also done—was a natural transition. He works in their geriatric medicine department, and he also joined TCU’s faculty when the medical school was started in 2018; he serves as the chair of clinical sciences. He had also been involved in teaching residents at JPS and Medical City Fort Worth.
He has three charges for those who are just starting out on their careers: physicians must consciously subjugate their own desires for the good of the patient; they have to recognize the unique role of the profession and the responsibilities it entails; and they should always practice with humility.
“We must realize we are no better than our fellow human beings and treat them with respect, no matter what the circumstances of a fellow human being are.”
Dr. Capper does not limit his teaching to the classroom; he marries his love of education with caring for the underserved most Saturdays when he oversees the student-run clinic at Beautiful Feet. As he works with students, he encourages them to make sure they have the right perspective when caring for their patients.
“My warning to the future of medicine is that we need to come back to more of a standard that is time immemorial,” he says. “We shouldn’t bend to the culture; we still need to hold true to ultimate or eternal values.”
Ultimate and eternal values drive Dr. Capper in all that he does. When he isn’t working, he has often spent time ministering to others alongside his family; years ago, when his children were growing up, they did family mission trips together every summer instead of family vacations.
He is incredibly proud of the people they have become, and whenever he and Dianne have the chance, they love spending time with their children, their children’s spouses, and their ten grandchildren, as well as close friends they have worked and served alongside over the years.
Looking back over his career, Dr. Capper is grateful for the path his life has taken.
“You have a relationship with people that exceeds that of any other relationships between people and a profession,” he says. “It’s not just contractual but covenantal; it’s about making a difference.”