Feature Article
By Allison Howard Hunter
This article was originally published in the January/February 2026 issue of Tarrant County Physician.
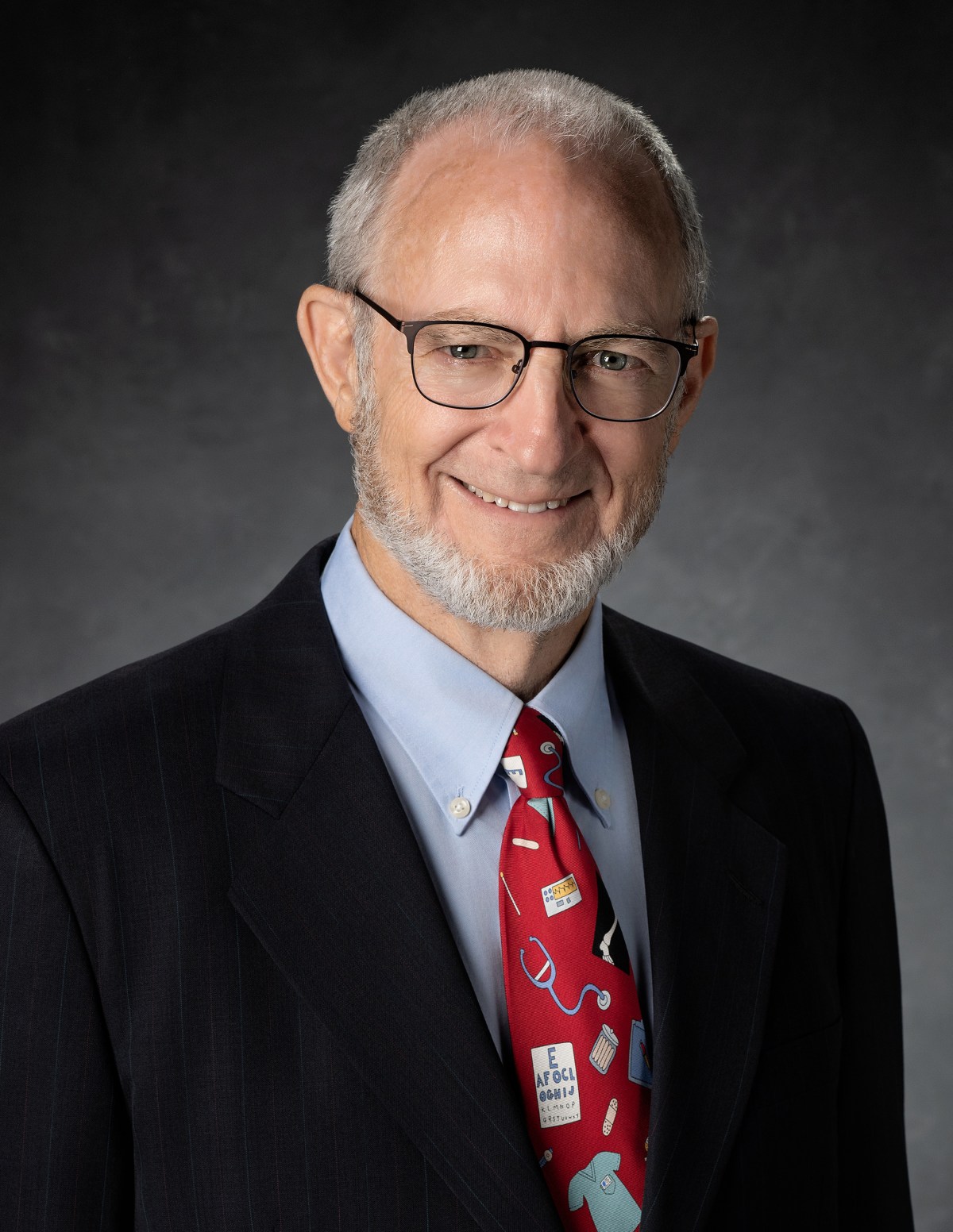
Dr. Cheryl Hurd, a psychiatrist committed to both clinical care and medical education, believes that organized medicine is the foundation that supports every other part of medical practice. But she’ll be the first to admit that she didn’t realize its importance early on.
“I was a student member of TMA, but I never did anything,” she says. The same was true during her residency in Arizona. But after years of participation, Dr. Hurd’s advice for medical students and residents is simple: Don’t just join—get involved.
When she returned to Texas and entered private practice, it was as the only psychiatrist in her medical group. Feeling alone, she rejoined TMA and immediately found connection in colleagues, committees, and a whole psychiatry track of support she didn’t know she was missing. “The camaraderie was huge,” she says. “I finally didn’t feel like the only one.”
Dr. Hurd’s involvement in organized medicine also offered practical benefits: TMLT insurance, CME funding, and—most importantly—the chance to advocate. Advocacy, she says, is what allows physicians to push back against excessive regulation, protect physician-led teams, and fight for the future of the profession.
She’s candid about the challenges physicians face. “Healthcare is regulated more than almost any other industry,” she says. Yet advocacy has delivered real wins: tort reform, increased medical education funding, and—critically for her field—expanded mental health funding in Texas even during budget-cut years.
“That’s why advocacy matters,” she says. “It protects us, it protects our patients, and it keeps our profession alive.”
And, as she found, those who advocate for you also have your back at the toughest of times, sometimes in ways that are less obvious than legislative wins. In 2020, when physicians were on the front lines of the COVID-19 pandemic and PPE was scarce, putting healthcare professionals at greater risk, Dr. Hurd was surprised to receive a box from TCMS.
“I opened it up and it was five hundred N-95 masks,” she says. “Just this whole box of N-95s. And then there was an email. It was from TCMS, saying, ‘Hey, we’re trying to help you.’ And they sent it to every single member; they sent every member a box because they wanted to protect us.”
Dr. Hurd credits that support as the reason she got even more involved, leading to her serving as our 2026 TCMS president. She saw in TCMS a reflection of her own ideals—a mission to care for patients, physicians, and the physician-patient relationship.
But it is the physicians like Dr. Hurd who give our medical society its heart, inform its values, and guide its vision.
“Dr. Hurd is the intelligent and compassionate doctor that you would wish to take care of your dearest loved ones,” says Helene Alphonso, DO, a friend and mentee of Dr. Hurd. “As a mentor, she nurtures lifelong learning at every level of medical education. She advocates for her patients and fellow physicians with countless hours and innovative solutions. . . . We can’t wait to see how her leadership in the Tarrant County Medical Society will shape the future.”
Though Dr. Hurd is now passionate about all things medicine, growing up, she did not want to be a doctor—or a teacher or a dancer or even a veterinarian (though she does have a major love for animals). No—at six years old, Dr. Hurd was determined that she was going to be a lawyer. She held on to this dream all the way through college, where she earned both a bachelor’s and a master’s degree in English from SMU, still convinced that law school was her next step.
It was during those years of study that Dr. Hurd met her husband, Howard. They had a good plan: he would go to medical school, and she would go to law school. Still, she decided to defer for a year because his education was taking him to Houston, while Dr. Hurd’s was taking her to Austin. As newlyweds, this separation was hardly appealing, and with law school only taking three years against medical school’s four, the choice was easy for her to make.
Dr. Hurd had planned to work in editing or proofreading for the year, but with a competitive job market and no connections in a new city, she had a frustrating lack of success. One day, she asked her husband if she could join him for his classes to give her something to focus on aside from the unfriendly job market, so he brought her along. She was immediately enthralled.
“A couple of weeks into his school, and I’m sitting there in the classroom taking more notes than he is,” Dr. Hurd says, laughing. “And I just thought, ‘Wow—this is fascinating. Why did I never study this?’”
Quickly, her decision was made—medicine was her future. In a short time, a passion grew into something she knew would sustain her in the years ahead.
Dr. Hurd and her husband were both accepted to Texas Tech’s School of Medicine, so they made the move to Lubbock. A couple of years later, Howard matched to a general surgery residency in Temple, Texas, so she transferred to A&M College of Medicine to complete her clinical rotations. When she graduated in 1998, she began her psychiatry internship at Good Samaritan Regional Medical Center in Phoenix, Arizona. Her training was unique—a joint internal medicine and psychiatry program that allowed her to combine the specialties that most interested her.
After her internship and four years of residency, Dr. Hurd was more than ready to begin practicing as a fully qualified psychiatrist. She and her husband knew they wanted to come back to Texas—the question was simply where they would land. Having their friends and family here was a huge draw for the young couple, but they were also motivated by positive legislation for medicine.
“With tort reform in 2003—that’s when I graduated residency—I was thinking it would really be nice to not have escalating malpractice costs,” Dr. Hurd says. “They’d still get money if I actually did something wrong, but the goal was that all the frivolous lawsuits would go away. And by and large, they have.”
They settled in Brownwood, Texas, where Dr. Hurd set up a psychiatry solo-practice collaborating with a larger organization of specialists. She was the only psychiatrist in the area, and she also consulted at the county hospital. At first this kept Dr. Hurd quite busy, but her practice slowed down after the financial crash of 2008. Soon she moved to Fort Worth, where she joined UNT Health Science Center and UNT Health, although her clinical assignment was at JPS. She later transitioned to Acclaim Physician Group when it was formed, and she stayed there until 2022. Throughout that time, her role grew from serving as the consult medical director to being the psychiatry program director and vice chair of education.
Though she was involved in education through TCOM and JPS, she maintained an active full-time practice. However, when she began serving as TCU Burnett School of Medicine’s psychiatry clerkship director, she stepped back from her role at JPS and joined Connections Wellness in a part-time role.
“At Connections Wellness, I still have a clinical job where I see patients and precept students,” says Dr. Hurd. “And then I had my role as psychiatry clerkship director. I do the behavioral health year-one lectures, clinical skills, and things like that. So, I’m all things psychiatry at the School of Medicine.”
Though Dr. Hurd treasures her role within medical education, she did not seek it in the early days of her career. When opportunities first arose in education, she turned them down in favor of focusing on her clinical practice.
“I thought, ‘No, I’m just going to go out and save the world one patient at a time,’” she remembers. “‘I’ll do clinic and just be a doctor, be a practicing physician. That’s what I was trained for.’ When I started at JPS, I just thought I’d be a psych consultant like I was at the county hospital down in Brownwood. So, I show up, do my orientation, and they’re like, ‘Here’s your team.’
“I went, ‘Team? What team?’ I had a resident, I had an intern, I had students. I just tried to base my precepting on some of the best preceptors I’ve had in my training. So that’s how I got involved and learned that I really loved it.”
Much like her discovery of medicine, Dr. Hurd considers this unexpected assignment another act of serendipity—one that was to her benefit, as it was (and is) for the many residents and medical students who have been under her tutelage.
Her colleague, Debra Atkisson, MD, has seen Dr. Hurd make a big impact both in education and practice throughout her career.
“I have known her for more than fifteen years and have observed her dedication to her patients and the medical students and residents she has taught,” says Dr. Atkisson. “She has provided our community and the state of Texas with outstanding education about psychiatry. . . . We are very fortunate to have Dr. Hurd serve as our president for Tarrant County Medical Society.”
Dr. Hurd has had variety in the roles she has held throughout her career, but they have all hinged on one overarching goal: supporting mental health for physicians and patients alike. This has involved making petitions both to TMA and the Texas Medical Board, being involved in mental health legislation through First Tuesdays, and serving on councils and boards supporting mental health—including TMA’s Physician Health and Wellness Committee, where Dr. Hurd served for the maximum nine-year term, including two years as vice chair and two years as chair.
Though progress has been made in mental health support and treatment, she sees that much more lies ahead.
“I want to continue to work on reducing the stigma and also try and get more involvement in the community itself to support and encourage and grow mental health access.”
But the problem goes beyond the average patients—physicians struggle greatly when it comes to accessing mental health.
“We’re the last ones to go seek help,” she says. “There used to be punishment for physicians with their licensure when they were under treatment. So, they didn’t seek treatment, or they felt like they couldn’t be honest about treatment. And there’s been a huge effort to flip that narrative and get physicians to understand it’s actually okay to get treatment, and this is thanks to both the TMA and the Texas Society of Psychiatric Physicians, after much work and many, many years.”
As she begins her term as TCMS president, Dr. Hurd does so with the goal of continuing this mission.
“One of my goals is to get the community more informed of opportunities for mental health support,” she says. “We are also trying to work on increasing access and bringing more behavioral health and mental health programs to the area.”
Those who know her believe Dr. Hurd will thrive in this role and ably utilize the opportunities it provides.
“I knew of her leadership at the Texas Medical Association, where she served on the Physician Health and Wellness Committee,” says Angela Self, MD, who has been friends with Dr. Hurd for many years. “She works tirelessly for her patients and for the practice of medicine. . . . She sacrifices many hours volunteering, advocating for the improvement of healthcare for physicians and patients across the country.”
As Dr. Hurd looks toward the future, she does so remembering the many physicians who have impacted her career. Carol Nati, MD, was a great mentor for Dr. Hurd, especially during her time at JPS. Dr. Atkisson encouraged her to get involved with TCU’s School of Medicine and Connections Wellness, and Greg Phillips, MD, helped give Dr. Hurd the drive she needed to get more involved with TCMS. Dr. Hurd credits these physicians—alongside many others, and her ever-supportive family— for helping her become the doctor she is today.
Though medicine always keeps her busy, Dr. Hurd loves spending time with her husband; their two children, Dawna and Perry; and their dogs (they always have several, and there is usually a rescue in the mix). If she has a spare moment, you’ll probably find her reading a book—all genres are welcome!—or joining in a multiplayer computer game that her husband got her involved in years ago. She’s now the only one in her family that plays, but through it, she has developed a network of friends spanning the globe.
“It’s kind of fun to have long-term friendships that are not based on just your circle,” says Dr. Hurd. “It gets us out of our comfort zones in those boxes we live in, where we only do things with people who are pretty much like us.”
Dr. Hurd is eager to widen her scope of friends and colleagues even further in the year ahead as she partners with physicians and other change-makers to make a difference for medicine in Tarrant County and beyond.
“I’m excited to see what we accomplish for medicine in 2026,” she says. “There’s a lot of work to be done!”