By Emma Freer
Originally published in Texas Medical Association’s January 2022 issue of Texas Medicine. It was republished with TMA’s permission in the March/April 2022 issue of Tarrant County Physician.
When Trey Moore, MD, started his career as a urologist in Fort Worth 26 years ago, he worked in a busy emergency department and his own private practice. In both settings, many of his patients weren’t covered by insurance and could only access stopgap care. At the same time, he was surprised by the dearth of opportunities for physicians like him to give back to their community by offering their services pro bono.
So, in 2011 he jumped at the chance to join Project Access Tarrant County, a then-nascent initiative of the Tarrant County Medical Society (CMS) that connects low-income, uninsured residents to specialty and surgical services provided by a network of volunteer physicians and facilities. Since its start, Project Access has served more than 1,700 patients and provided more than $14.5 million in donated health care.
Dr. Moore especially likes the program’s focus on surgical care, which is unique in the world of health care safety-net programs. Given his specialty, many of his neediest patients – such as those suffering from large kidney stones that cause recurring, and sometimes disabling, infections – require surgery to recover fully.
“Every [pro bono service] makes a difference, whatever we do, but [Project Access is] particularly helpful because so many of these patients – until they have a surgical resolution – are stuck in a vicious cycle of not being able to go back to work and cycling in and out of emergency rooms,” he said. “It’s a big stress on the patients and their families, and it’s a big stress on the system.”
But relieving that stress would not be possible without ongoing financial support.
Project Access is one of several long-standing recipients of the Texas Medical Association Foundation’s Medical Community Grant program, which accepts applications from county medical societies and alliance chapters for up to $7,500 in matching funds to support unique community health improvement initiatives. The separate Medical Student Community Leadership Grants program accepts applications from TMA medical student chapters for up to $3,000 thanks to a fund established by Houston pathologist Roberto J. Bayardo, MD.
For more than two decades, TMAF’s grant programs have helped the Family of Medicine tackle the state’s most pressing health care concerns at the local level. Many grantees, including Project Access, have received funding over successive years, which allows for continuous programming. Physicians like Dr. Moore say this is especially important in Texas, which has the highest rate of uninsured residents in the nation.
Not only do the grant programs connect patients to life-changing care but also they honor TMA’s mission to stand up for Texas physicians by providing them with resources to create solutions to local health challenges and by reinforcing physicians’ trusted leadership in the community, says TMA Foundation Executive Director Lisa Stark Walsh.
“Our goal is to remove the obstacle of resources for members to do what they feel is necessary in their communities,” she said. “Medical Community Grants give physicians an opportunity to chip away at long-standing, intractable problems over the long term and to demonstrate their advocacy for the health of all Texans.”
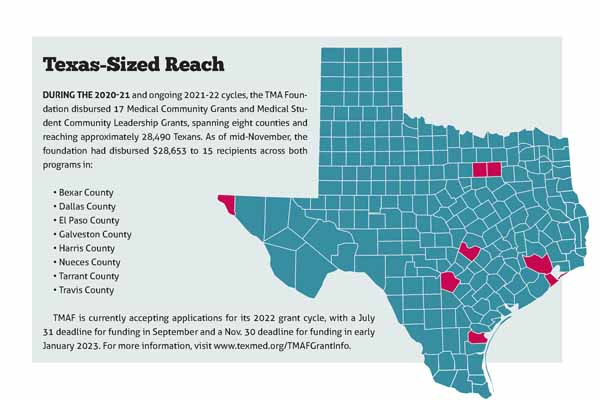
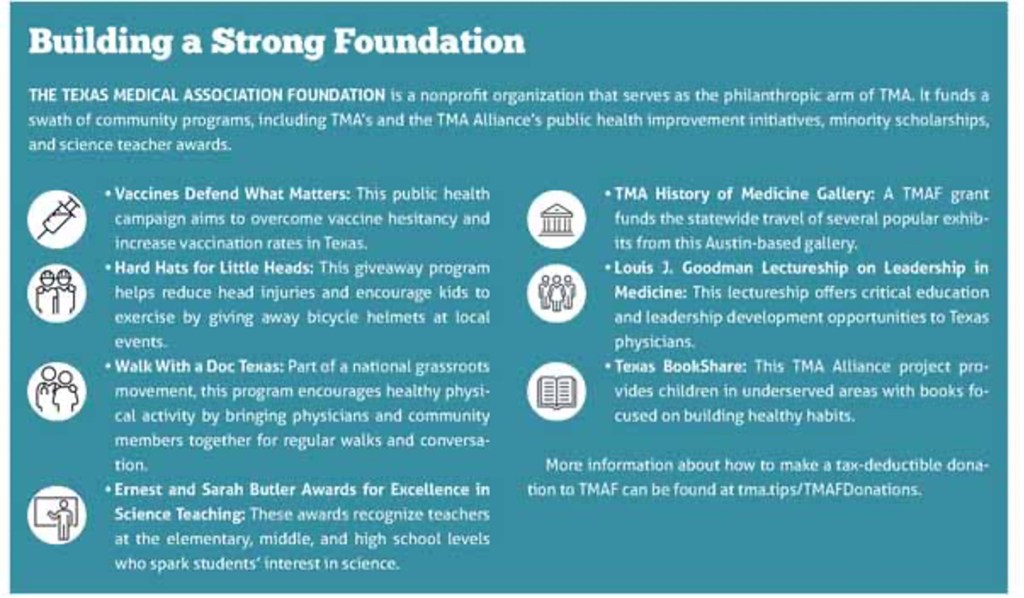
Originally founded in 1966 as the Texas Medical Education and Research Foundation, TMAF is a separate, nonprofit entity that serves as the philanthropic arm of TMA. Since 1998, the Medical Community Grant and Medical Student Community Leadership Grants programs have disbursed $891,931 across more than 200 such grants to support myriad community health improvement programs all over Texas, ranging from vaccine clinics and border health services to breast cancer screenings and kids’ bicycle helmet giveaway events.
Houston neonatologist and TMAF Board President Michael E. Speer, MD, is passionate about growing the foundation’s endowment so it can offer even more grants that support Texas physicians and their patients. “If you look at the most successful colleges and charities, the best ones spend very little on themselves and most of their endowment on supporting the organization,” he said.
This growth mindset has paid off. In recent years, TMAF has fielded increased demand for the grant programs from county medical societies, alliance chapters, and medical student chapters. As a result, the upcoming application cycle will include a new focus area of physician health and wellness. This expansion stems from the success of a recent TMAF initiative, Caring for Physician Healers: Mental Health and Wellness Resources During COVID-19 Fund, which helped seven county medical societies launch or extend physician health and wellness initiatives during the ongoing pandemic. (See “Self-Investment: Physician Wellness Programs Bolster a Beleaguered Workforce,” November 2021 Texas Medicine, pages 22-25, http://www.texmed.org/Self-Investment.)
By harnessing the expertise of medicine to help address a community health problem, the TMAF grant programs complement the work of the association and represent the best of organized medicine, says TMA President-Elect and TMAF board member Gary Floyd, MD.
“Anyone in practice will find things that need to be changed,” he said. “When you’re alone or in a small group, you’re just a small voice yelling into the wind with very little result. When you join into organized medicine, particularly with TMA, you have [more than] 55,000 voices, and people tend to start listening.”
Physician-driven results
Tarrant County Medical Society received its eighth TMAF Medical Community Grant in support of Project Access in 2021. The program’s organizers say it is a prime example of what physicians can accomplish working together to solve an entrenched community health problem. Tarrant CMS was inspired by the Dallas County Medical Society’s now defunct Project Access initiative, which focused on primary care. Given Tarrant County’s robust network of free and income-based primary care clinics, Tarrant CMS decided to gear its own Project Access initiative toward specialty and surgical care since that’s where the need was most acute.
Tarrant CMS Executive Vice President and CEO Brian Swift says Project Access runs on a shoestring budget that belies its impact. Patients are largely members of the working poor, and many are undocumented immigrants. They don’t qualify for Medicaid but typically don’t earn enough to afford private insurance, leaving them without coverage and beholden to emergency departments for symptom management. Without care that addresses the root cause of their medical problems, however, they are often robbed of their livelihoods – and sometimes their lives.
By providing specialty and surgical care to eligible Tarrant County residents, the initiative not only helps patients resume healthy lives but also saves area hospitals tens of thousands of dollars in emergency department costs. “These patients don’t have access anywhere else,” said Stuart Pickell, MD, Project Access’ medical director and an internist-pediatrician in Fort Worth.
Although physician volunteers provide specialty and surgical care, Project Access still requires funding to fulfill its mission. “Free isn’t free,” Mr. Swift said.
As with previous awards, the county medical society used the TMAF funds to offset the costs of its annual patient database subscription. “Data management does not come cheaply, so we really depend on that [funding] to be able to manage our Project Access database,” Mr. Swift said.
The grant-funded database – which Dr. Pickell describes as “essential” – allows staff to determine patients’ eligibility, which helps ensure Project Access is distributing its limited resources as judiciously as possible, and to track their care, including the donated value of medical services and administrative costs. In this way, the grant helps Project Access obtain more funding by quantifying its positive impact and cost savings.
Armed with the database, staff can focus on serving patients – and the broader community. Typical cases include a woman with cervical cancer who would have died without surgery, leaving her young children orphans; a construction worker with a hernia that kept him out of work; and a patient with osteoarthritis that had nearly disabled her until surgery allowed her to resume a productive life.
The Project Access model not only unburdens its patients and their loved ones from medical crises but also often allows them to return to work. This can be transformative, Dr. Pickell says, because a job offers the possibility of long-term health care access through employer health insurance.
After a decade of success, staff are now working on growing the program. With more than 500 volunteer physicians across numerous specialties, including ancillary care, their attention is focused on the limiting factor of operating room space and other facility needs. By renting such space, rather than relying on the whims of donors, Project Access can increase its patient volume.
Physicians would welcome such a change. “It’s such a gracious group of people,” Dr. Moore said. “They’re so grateful to get help. In a selfish way, it’s a great group to treat.”
Project Access also is keen to expand, both to meet the community need and to highlight the work physicians do every day to serve their patients. It’s supported in this endeavor by TMAF’s Medical Community Grant program, which allows physicians to spearhead solutions to the problems they’re facing on the ground.
“That’s why it’s so important for the foundation to continue doing what it does,” Mr. Swift said.
An engine for innovation
Another repeat recipient, in this case of the TMAF Medical Student Community Leadership Grants program, the annual HOPE Health Fair in Galveston tackles a community health challenge while also providing medical students with the opportunity to fine-tune solutions over the long term.
The University of Texas Medical Branch (UTMB) TMA Medical Student Section chapter hosted its fifth annual event in November thanks, in part, to its fourth annual TMAF grant award. The fair connects approximately 250 uninsured Galveston residents – around a quarter of whom are homeless – to vaccinations, health care screenings, meals, and educational resources through the St. Vincent’s Student Clinic at UTMB. It also serves as a critical outreach opportunity in Galveston County, where 17.4 percent of residents under age 65 lack health insurance, according to the U.S. Census Bureau.
“We’re just catching ships in the night, people who frequently never have access to health care,” said John W. Davis, one of the event’s organizers and a third-year medical student at UTMB who also is pursuing a PhD.
The HOPE Health Fair received a $3,000 Medical Student Community Leadership Grant from TMAF in 2021, which covered about 40 percent of the overall cost. Without it, organizers would not have been able to host the event. “It’s very helpful for us to get this grant each year,” said Jenna Reisler, a third-year medical student at UTMB and an event organizer.
In addition to providing critical funding, the grant also has spurred innovation. Because the organizers are repeat recipients of the grant program, they take pains to improve the event each year. In 2021 they used the award to offer rapid COVID-19 testing and screenings for sexually transmitted infections, including HIV and hepatitis C.
By offering screenings, the organizers not only help attendees detect any debilitating illnesses they might have contracted but also prompt them to return to the student clinic to get their results and receive treatment. Once attendees have made the jump from the health fair to the student clinic, they can receive treatment for underlying health problems, such as diabetes and hypertension, and start to build patient-physician relationships.
In this way, the health fair functions as a kind of benevolent Trojan horse, linking Galveston’s most vulnerable residents to health care for years to come. “It’s a way to show people that we care about them,” Mr. Davis said.
Global reach
Located in a top U.S. county for refugee resettlement, the Baylor College of Medicine (BCM) TMA Medical Student Section chapter and the Houston nonprofit Alliance for Multicultural Community Services have used the TMAF Medical Student Community Leadership Grants program to host the BCM-Alliance Refugee Health Fair. The annual event helps refugees navigate the local health care system – and provides medical students a glimpse at global health in action.
Like the HOPE Health Fair, the BCM-Alliance Refugee Health Fair aims to serve as a conduit for attendees to long-term health care access. At an upcoming event scheduled for this spring, student volunteers will distribute hygiene kits – including soap, hand sanitizer, masks, and health care resources in multiple languages – via a COVID-19-safe drive-thru. Attendees also will receive basic preventive health screenings and flu vaccines from local free and income-based clinics.
Although refugees can access Medicaid for up to eight months upon their arrival in the U.S., they are expected to secure private insurance afterward. This is a complicated process that can quickly fall to the bottom of a refugee’s to-do list, overtaken by tasks such as learning a foreign language, securing a job, and familiarizing oneself with the local public transit system. But the BCM-Alliance Refugee Health Fair aims to smooth attendees’ search for health care by introducing them to the Alliance and area clinics.
“Ultimately, even if these patients don’t stay on with these clinics, they at least have a starting-off point to return to if they develop a medical issue in the future,” said Avery Haugen, a fourth-year medical student at Baylor and one of the event’s organizers. “It really alleviates a lot of the stress of those first steps.”
The Baylor TMA student chapter will use its latest TMAF grant – its fifth – to print promotional flyers, purchase hygiene kit supplies, and furnish volunteers with personal protective equipment. The grant, which accounts for nearly all of the event’s budget, is critical to its success.
“This event is really not possible without the help from the TMA Foundation,” said Chris Wong, a fourth-year medical student at BCM and another event organizer.
In addition to educating refugee attendees about the local health care system, the event also serves as a critical learning experience for the medical students involved. Both Ms. Haugen and Mr. Wong are interested in global health, which is partly what prompted them to get involved with the fair.
“The event was really my first exposure to the idea of refugee health [and] the very specific health disparities that immigrants face, especially in our very complicated health system,” Mr. Wong said.
Similarly, Ms. Haugen sees the event as a unique opportunity to learn more about global health while studying medicine in Houston – and largely prohibited from international travel by the ongoing pandemic.
“For us, the refugee health fair is a really unique example of a way to promote global health on a local scale,” she said.


