Cook Children’s pediatrician and TCMS member Dr. Jason Terk shares the tragic way one of his young patients was impacted by COVID-19, and why it is critical to protect the health and wellbeing of children by getting vaccinated.
COVID-19 Positive cases: 441,134
COVID-19 related deaths: 5111
Recovered COVID-19 cases: 373,903
Data from Tarrant County Public Heath’s (TCPH) report of COVID-19 activity in Tarrant County updated Thursday, January 13, 2o22. Find more COVID-19 information from TCPH here.
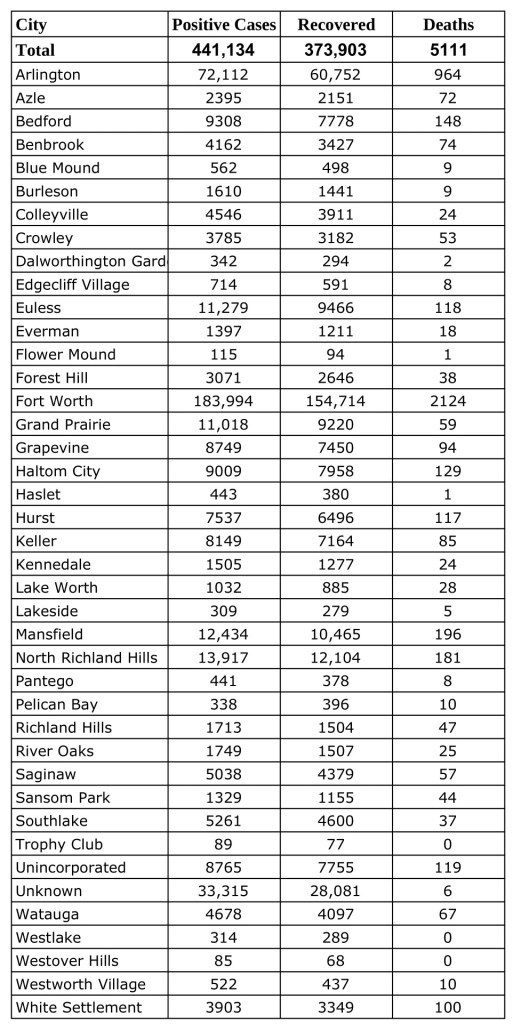
*These data are provisional and are subject to change at any time.
Deaths and recovered cases are included in total COVID-19 positive cases.
by Allison Howard
All too often, struggles with our health bleed into other areas of our lives. “Melanie’s” hernia did not just cause her stomach pain and inflammation – it stopped the mother of three from playing soccer with her children. It made her struggle with depression and lack of motivation. It made her worry about the future.
Melanie had to go to the ED several times because the pain became severe, and she worried that her condition would become worse. Her children were anxious about their mother’s health, and she was concerned about them – her youngest is only one year old.
She sought care at Cornerstone Health Network, and it was there that Melanie was referred to Project Access. At that point she was relived – there was hope for the future. Melanie knew she would receive the care she needed, the care that she could not otherwise access due to lack of resources.
Melanie was referred to Project Access volunteer Dr. Mohamad Saad, who agreed that she needed surgery to repair the hernia. Dr. Saad performed her surgery at Harris Southwest Hospital, and anesthesia was provided by US Anesthesia Partners – Southwest Division.
Now, Melanie is again playing with and taking care of her children without pain. She is grateful to everyone who made this possible – from Project Access to Dr. Saad and his staff – because it has given her the opportunity to live a better life.
One of the things that makes Melanie happiest is knowing that it doesn’t stop with her – that many other people have also received critical care through these services. She shares her thanks for the help and genuine care that is extended to Project Access patients.
By Shanna Combs, MD
This piece was originally published in the January/February 2022 issue of the Tarrant County Physician. You can read find the full magazine here.

Welcome to 2022! This is going to be our year. Things are going to be better. So long, COVID . . . Oh wait, maybe not. Doesn’t this all sound a little too reminiscent of the start of 2021? As I write this, we are in the beginning stages of a new variant, Omicron. There is still much we do not know about this variant, and hopefully, by the time you are reading this, it will have turned out to be not as bad as the last one.
Thinking back to the start of 2021, we were elated to have new vaccines to fight off and end the COVID pandemic. Many of us in healthcare were racing to sign up to get our shot and show it off on social media. We finally had some armor to protect us in this fight, and soon enough it would be available to protect our families, friends, and patients. Yet the conversation quickly turned to, “It was made too quickly,” “You can’t mandate that I get the vaccine,” “I am healthy; why do I have to get the vaccine?” or “It is all fake news.” So now, here we are, entering the “terrible twos” of the COVID pandemic. If there is one thing that has been demonstrated during the COVID pandemic, it is that the innate trust in physicians, medicine, and science is, unfortunately, no longer so automatic. We as physicians must continue to be voices for science and for medicine who, at the end of the day, want the best health outcomes for our patients.
As we enter the terrible twos of the pandemic, I encourage my physician compatriots to be the voice that our patients and our society need to hear. Whether that is in your day-to-day interactions with patients, conversations with family and friends, or in public venues, we must continue to be the voice of medicine. Ways to amplify that voice exist within our own county, state, and national medical society. Those of us in medicine often focus on what makes us different, but now more than ever we need to focus on what brings us together.
We are all tired and exhausted from this fight, and more than once I have heard others as well as myself say, “Can’t we just go back to how it used to be?” Unfortunately, I hate to say, COVID is with us for the foreseeable future. Yet, those of us in medicine went into this field for a reason. For me, that reason always comes down to my patients. I want to provide the best care to optimize the health and well-being of my patients. During these terrible twos, I call on my colleagues to remember why you embarked on this journey of medicine, and when you see a colleague struggling, help them to remember why they came to this profession. Not only can we be the voice of medicine to our patients, but we can also be the voice of support and camaraderie for our fellow physicians.
As we embark on this new year, I want to say that I support you as a fellow physician, and I look forward to the amazing work that you all contribute to your patients and to our society. Thank you for what you have done and what you will continue to do.
by Allison Howard
This piece was originally published in the January/February 2022 issue of the Tarrant County Physician. You can read find the full magazine here.

When Dr. Shanna Marie Combs was a little girl, she knew when she grew up that she wanted to be a doctor and a ballerina. Not a doctor or a ballerina – she wanted to dance and practice medicine. So that’s what she did.
The combination might seem odd, but when the OB/Gyn, who is a self-declared science nerd, ended up seeing multiple orthopedic surgeons throughout her childhood to manage dance-related ankle complications, the interest came organically.
“I was seeing orthopedic surgeons at the age of 12,” Dr. Combs says. “They all wanted to operate on me, and I would push back and be like, ‘No, I need another option.’” She laughs as she remembers her juvenile determination. “It came to the point I would have orthopedic surgeons print out journal articles for me.”
While her interest in medicine only grew as she did, Dr. Combs realized that she should pursue dance first if she wanted a real shot at both of her passions. After all, professional dancers have limited careers, and Dr. Combs was facing an even bigger challenge with her stressed ankle.
“I used to joke that medicine was my backup career for ballet,” Dr. Combs says with a grin.
She pursued a Bachelor of Fine Arts in ballet at TCU while taking all the necessary prerequisites to apply for medical school. Even though she wasn’t ready to take that step, she wanted to be prepared. It was a hectic time – she always took the maximum number of hours and had to take her science classes in whatever order they were available to work them around her dance classes.
After graduating, Dr. Combs joined the Ballet Theater of New Mexico in Albuquerque, where she had danced in high school. While there her life revolved around ballet – she performed, worked with students, and even managed the studio’s front desk.
Dancing was fulfilling, and Dr. Combs looks back on that time fondly. She created a special bond with her “ballet ladies,” one that holds strong these many years later. Still, the time had its challenges. Money was tight, and she ended up taking another job as a physics lab tech at a community college.
Dr. Combs was also physically feeling the impact of constantly dancing, so after a couple of years of performing professionally she decided it was time to move on to medical school. It was at that point that she hit a snag in the plan; she didn’t get accepted to the places where she had applied.
“I kind of had to have a real heart-to-heart with myself as to whether or not I actually wanted to do this again,” Dr. Combs says. “But ultimately, I was like, ‘No! You want to be a doctor.’ So I retook my MCATs and applied broadly and got in.”
She attended medical school at the University of New Mexico. Based on her childhood, she had thought she might go into orthopedics or perhaps pediatrics, but when she began her third-year rotations, she found she was drawn to obstetrics and gynecology. No one was more surprised than she was.
“I said I would never do OB/Gyn as a first-year med student, and here I am, as an OB/Gyn,” Dr. Combs says. “I did not understand the scope of what an OB/Gyn does, and probably my first day on the rotation I was like, ‘Oh, I kind of like this.’ So I fell in love with the field.”
It has been her passion ever since. She completed medical school in 2008 and began her residency in obstetrics and gynecology at JPS. She finished the program in 2012 and then began working for JPS Health Network in private practice as well as in education for the residency program.
Her love for teaching and education led to her involvement in the curriculum development of the TCU and UNTHSC School of Medicine, and she ultimately became the OB/Gyn clerkship director at the new medical school. Though Dr. Combs recently left that position, she is continuing to work with students; it’s one of her favorite roles as a physician, to prepare the next generation of doctors.
“When you work with students, I always say you can learn what to do and what not to do, and I always wanted to be somebody where they hopefully learned what to do in working with me,” Dr. Combs says. “I’d always loved teaching, so once I discovered that, oh, I can teach in medicine too, I kind of continued that in residency working with medical students and residents who were below me as I moved up and ultimately into education and working with students.”
In spite of her focus on education, Dr. Combs has maintained an active private practice. Last year she transitioned to Cook Children’s Physician Network, which has been an amazing opportunity to marry her love of pediatrics and OB/Gyn, two fields of medicine that rarely intersect.
“A lot of gynecologists won’t see kids younger than 16 or 18,” Dr. Combs explains. “There was definitely a need; it’s totally blown up. And I love it. I can’t tell you how many times women have brought their daughters and been like, ‘We’re so glad you are here.’”
“[Dr. Combs] has taken on the awesome task of advocating for female teen and young girls’ health,” says Dr. Hannah Smitherman, a pediatric emergency medicine physician who is one of her colleagues at Cook Children’s. “It’s a niche that many shy away from . . . Teens are struggling with the stressors of a rapidly changing and conflicted world. Dr. Combs is there to help support these children, soon to be adults, through their often very personal medical issues.”
Currently she sees any patient between the ages of 0–22 that needs gynecological care, but the bulk of her practice is made up of teenagers. “I love taking care of my little ladies,” Dr. Combs says. “I try to provide a very safe place.”
Recently, after displaying quite a bit of anxiety during her appointment, one of her young teenage patients came out to Dr. Combs as lesbian when they talked privately. It was something she had been afraid to tell anyone.
“As they were leaving, the patient kind of hangs back a little bit and she’s standing next to me,” Dr. Combs says. “And I’m like, ‘What’s up?’” Her voice is hushed as she reenacts the moment.
“And she said, ‘Can I give you a hug?’ My heart just broke. I just got the impression that she felt heard and supported . . . Stuff like that – it’s the best part of the job.”
Dr. Combs says there is one simple answer when it comes to organized medicine: “Do it!”
“As a medical student, I got involved in the New Mexico Medical Society and the AMA as well, and I remember talking with colleagues and fellow students,” Dr. Combs says. “They were like, ‘Ugh! I don’t want to deal with that stuff.’”
While she understands the hesitation physicians might feel, especially those just beginning their careers, she believes that it is critical for them to be involved in anything that impacts medicine.
“Am I a businessperson or a politician? Absolutely not,” Dr. Combs says. “Would I rather just practice medicine? Absolutely! But all those outside influences affect how I can practice medicine, so I’ve always wanted a seat at the table to kind of influence those decisions and choices.”
And if you feel underrepresented by an organization, Dr. Combs believes that is all the more reason to get involved.
“You can stand on the outside and throw stones and say, ‘They don’t speak for me,’ or you can say, ‘They don’t speak for me; I need to join that organization.’ Because the only way it’s going to change is if more membership gets involved.”
Dr. Combs tries to encourage medical students to participate just as some of her mentors encouraged her. One of those mentors, Dr. G. Sealy Massingill, who is an OB/Gyn practicing in Fort Worth, interviewed Dr. Combs when she applied for a JPS residency spot, and when she joined the program, he suggested that she participate with TMA and TCMS.
“I encouraged her to seek out opportunities in the community and feel grateful she chose to become involved,” Dr. Massingill says. “Her commitment to equity, diversity, and access to care have been drivers for her.”
Several years ago, Dr. Combs participated in TMA’s Leadership College. Since then, she has served on the TCMS Women in Medicine Committee and Publications Committee, and on the state level, the Membership Committee and Maternal Health Congress, as well as one of the AMA alternate delegates.
Now, she is ready to lead TCMS as she begins her term as the 2022 president. Dr. Demequa Moore, who is also an OB/Gyn taking care of patients in Fort Worth, says one of Dr. Combs’ greatest strengths is that she is driven by her deep care for others. “[She] has always practiced with empathy and compassion,” Dr. Moore says. “She continues to seek opportunities to learn and improve the health of her community.”
As Dr. Combs looks back over her career, a physician of particular influence comes to mind: the late Dr. Tracy Kobs. Dr. Kobs worked with JPS residents in the operating room when Dr. Combs was in the program, and she strives to emulate him as both a physician and educator.
“The more I learned about him over time, the more I respected him,” Dr. Combs says. “Operating, you want to get in, you want to do the job correctly, and you want to get out. And so when you’re working with learners you have to be very patient because they’re learning, and he never got frustrated or upset when things were taking too long or anything like that. He was always so patient . . . with the breaking down of steps. And even working with students now, teaching them how to do just basic knot tying and suturing, a lot of the mechanics I learned from him I bring to teaching with students.”
She is grateful for the cheerleaders she has had along the way, and her parents have been chief among them. They supported her at every step she took and challenge she faced.
At one particularly memorable moment, the family was driving back to Texas from Colorado when Dr. Combs found out she had passed her board exams. Her mother insisted that they had to celebrate immediately, so they pulled the car over so they could dance for joy.
“I love my parents,” she says, a big smile crossing her face. “I have to say, I’m very blessed.”
When she isn’t busy teaching, seeing patients, or attending meetings, Dr. Combs enjoys traveling with friends and family or spending time with her dogs, Duke and Poppy, and her partner, Mike Bernas.
While she has enjoyed her varied career and life experiences thus far, Dr. Combs looks to the future with anticipation because she sees it centered around her work as a physician, something that over the years, she has realized is more than just a passion.
“At the end of the day, I call it a calling,” Dr. Combs says. “You know, you hear people talk about their calling to ministry and things like that, but to be a physician has always been what’s at the center of me.”
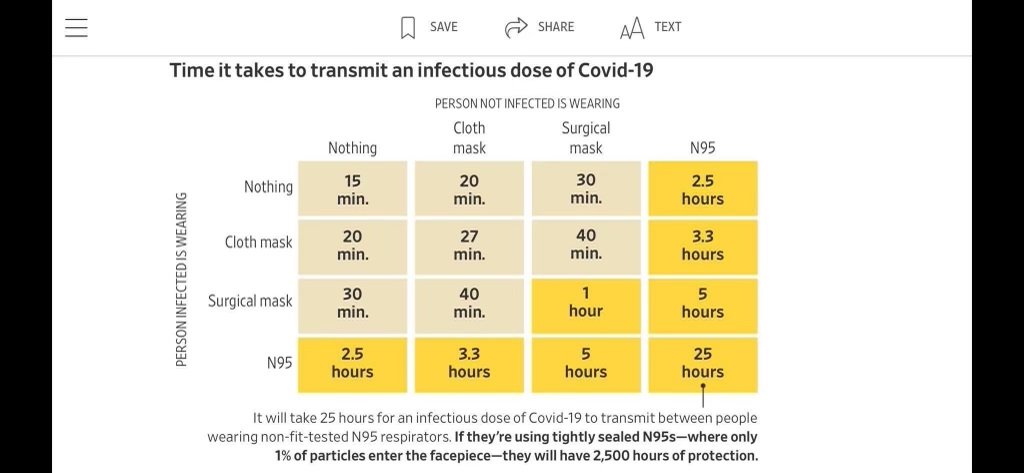
As the number of COVID-19 cases continue to rise in North Texas, the importance of protective measures also increases.
In the below North Texas Medical Society Coalition video, Fort Worth physician Dr. Robert Rogers, who is also part of the Tarrant County Medical Society, explains the different levels of protection provided by cloth, surgical, and KN95 masks, and how those differences impact his own decisions.
For more information on the transmission rates/mask types Dr. Rogers mentions in the video, please refer to the below chart:
By Shanna Combs, MD
This piece was originally published by TMA on Blogged Arteries, a forum for physician opinion and commentary, on February 28, 2018.

I spoke with a young woman recently who is working on her application to medical school. She had the same excitement and nervousness regarding the application process that I had when I began my journey into medicine. Unfortunately, I was disheartened to find out that she had spoken to many physicians who had tried to talk her out of going to medical school and pursuing her dream of becoming a physician.
I chuckled with her saying I had experienced the same thing. Unfortunately, she was even starting to question her desire to be a physician.
What happened to our field? Why are those of us in practice frequently found telling prospective students not to join our path and seek another one with better pay, better work-life balance, and more appreciation?
Are there frustrations with the health care system, insurance, and electronic health records? Yes.
Do we work long hours with minimal acknowledgment of our dedication? Yes.
Do our years of study and practice get dismissed for the more vaunted Dr. Google? Yes.
Do we sometimes forget why we even became a doctor? Yes.
Do we also have the privilege to help patients through some of the most exciting as well as difficult times in their lives? Yes.
I find it an honor to be a physician. Do I deal with all the above concerns mentioned? Yes.
What happened to our field? Why are those of us in practice frequently found telling prospective students not to join our path and seek another one with better pay, better work-life balance, and more appreciation?
However, when a patient says thank you for my support during a difficult diagnosis, or I see the tears of joy on the face of a new mom as I hand her her baby for the first time, I remember why I became a doctor.
You can read the full article here.
Shanna Combs, MD, is an obstetrician/gynecologist practicing in Fort Worth. Currently, she is serving as the 2022 president of the Tarrant County Medical Society.
by Angela Self, MD
This piece was originally published in the November/December 2021 issue of the Tarrant County Physician. You can read find the full magazine here.

The church bus let me off in front of the house. It must have been after a Wednesday evening service because it was dark. I started to walk toward the house when I heard “Angela, Angela.” It was my mom quietly calling to me from her car across the street, my little sister and brother in tow. I did not know at that moment that my dad was inside the house wreaking who knows what kind of havoc. My parents had been separated for a couple of years after my mom had all she could take of his drunken rages and unthinkable actions. One time we returned home to this very house in Oak Cliff, Texas, to find all of our windows broken out and a note on the kitchen wall (held there by a large butcher knife).
Let me back up for a minute. My dad was a brilliant man who had a heart of compassion and was an excellent teacher and patriot – when he was sober. The problem was that we rarely saw him sober in my early years. The thing about kids and their parents is, no matter how messed up a parent is, the trauma of losing them is greater than the pain endured by any disease or affliction they bring with their presence. For several years I would ask my mom if “Daddy” knew where we were and if he had called. I was sure that he just couldn’t find us. This feeling only got worse when we moved out of state. My mom met another man, and I knew he was there to stay when she told me that she was pregnant. That was one of the saddest days I can remember. I did not even know what abortion was at the time, but my mom could not afford to travel to California to get one (the year was 1973). I would not see or hear from my biological dad again until I was 19 years old.
One thing I knew was that I could not let my new little brother grow up without a dad. The pain of that loss was all I could bear as a child and I could not let another child, my brother, suffer in that way. So I kept quiet in the midst of abuse for years. I knew that I had to because mom would leave, and she would not be able to support us without him. I also knew my little brother would be as devastated as I was when I lost my dad. Yes, my stepdad was also an alcoholic. Both of these men have passed, my dad at 53 years of age and my stepfather at 69. I was at my stepfather’s bedside after the stroke that was likely a result of years of alcohol and tobacco use. He and my mother had divorced years earlier, thank God. I had forgiven everything and kept in touch, hoping he would find the same self-forgiveness and peace that I had found at 19 — you see, he also grew up as a child of abuse.
My mom was a little checked out (okay, a lot checked out) during the “Vegas years.” Though my stepdad was able to do a lot of construction work to support us, my mom struggled with a different addiction. My mom, who has likely never really been drunk or high, was a gambling addict. What does an abusive stepdad do when he wants the freedom to abuse his step kids? He tells his gambling addict wife to go to the casino and even gives her money for the little adventure. As soon as I was old enough to physically get out of the house, I would run away, stay out all night, miss school. My mom would ask me for years to come why I just spun off the rails at about 15 years old. She was concerned about my behavior and sent me to stay with my aunt in New York one summer and then for a semester in 9th grade. I met a boy there; he was cute. Right after I graduated from high school, I continued staying out all night. Mom told me that if I stayed out all night one more time, I could pack my bags and take them with me. I took Mom up on that offer, probably that day. I bought a bus ticket to New York (at 17) and informed the cute boy that I was coming to stay with him.
I worked as a dental assistant to help us pay the bills; there weren’t many as we mainly lived with his parents. Sadly, he also struggled with some issues that hit a button with me and led me out of the relationship ten years after I met him. I am grateful for all that I learned from his family; I did not really know what family was supposed to look like until I spent time with his. They were wonderful people who taught me things I had not learned at “home.” Do not misunderstand, my mom loved all of her kids very much, but she was dealing with her own childhood and adult struggles which took the focus off of anything other than keeping us physically safe (which would only happen while we were in her sight). Now I was an adult, out on my own, volunteering with my ambulance corps, working as a surgical dental assistant, going to college – just in a very unhealthy relationship. But what was a healthy relationship? It would be years before I knew, if I actually do know. We will leave my relationship struggles between me and my very capable counselor. Let’s get back to the casualties of war.
The pain of that loss was all I could bear as a child and I could not let another child, my brother, suffer in that way. So I kept quiet in the midst of abuse for years.
My mom and stepdad moved back to Texas. It’s funny how unsustainable it is when you tell your husband that you’re making the mortgage payment and you’re really putting it in the slot machines. It doesn’t work well with car payments either. They had an opportunity to buy a small home on a pretty lake near Caldwell, Texas. It was the town where we had gone to visit my grandparents when I was a kid. Things were seemingly okay with my mom, stepdad, and youngest sibling, my half-brother. Then things got rocky between my mom and stepdad, and my little brother dealt with the breakup by running with a crowd that was likely not the best. By the time he approached his teen years he had dropped out of high school and had started having kids. I remember his first daughter being born when I was in med school. He and his girlfriend began having problems and drugs entered the picture. At some point one of those drugs was meth. My mom has spent so many years trying to make up for the years lost with her oldest three kids by being a doting mom to her youngest and to his kids. At present my brother still struggles with meth. His oldest daughter, who ran track and got many awards before graduating from Caldwell High School, is now an addict who might not be alive as I write this. I really do not know. I am not allowed to mention my youngest brother to my other family members (except Mom) as we have all lived too many years waiting for that phone call from the police, hospital, or morgue.
You can take so much and then you just check out due to helplessness in the situation. We have all been casualties of addiction of various sorts, yet we fight on. My sister is a very good nurse and has been the best mom to her college student daughter. My sister does not drink or dabble with any of the substances that wrecked our family. My brother (the clean one) has a sheep farm, is a carpenter, a loving husband and father, and has also kept his house clean from any of the things that wrecked our lives. I am here writing this article, hoping my mom will not be too hurt as she is doing the best she can to try to save the life of her granddaughter this week. Literally, doing whatever she can to get her arrested so that she will not die in a drug house (weighing about 100 pounds, covered in sores, mind almost gone, and threatening to “fix herself” in her own way). Oh, don’t worry about the resources available – my niece has already been visited by the police and MHMR this week. There is nothing they can do.
The thing about meth is that it does not take its victims all at once; it slowly makes them and everyone in their lives casualties every single day. I wish I could give a hotline or support group info, but the only thing that I can do is pray. And I do, we do, pray. We have all come to terms with what addiction has done to our lives. We have made peace with the actions of others and regret how our own actions have hurt those around us, but we continue on in the midst of a bad dream and find joy in any area that life offers. As you go out today, remember that there is not a specific background that defines a physician, or an individual. Often, we assume that doctors only come from privileged environments, but many of us have a different story. Yet, I am the sum total of what a physician is, and so are you. We are changed, we are impacted, but we are not defined by our pasts. You never know who around you is a fellow casualty of war, doing their very best to enjoy one day at a time. God bless you all – it has been my honor to serve as your president.
Pediatrician Dr. Jason Terk recommends making careful choices as we begin a new school year while the Omicron COVID-19 variant rises in North Texas.
“Make sure you make your choices wisely about who you are gathering with,” he said. “And make sure you are gathering in safe ways.”
For more information, see the below video from WFAA:
Read WFAA’s full update on North Texas schools here.
Have questions about socializing in light of the rising COVID numbers that have impacted holiday plans for many, including several local restaurants who had to temporarily close their doors? Check out Fort Worth physician Dr. Gregory Phillips’ interview with Lili Zheng of NBC5 to see what he has to say on the topic:
You can read the full article here.